Total Knee Replacement
INTRODUCTION
The knee is essentially made up of four bones. The femur or thighbone is the bone connecting the hip to the knee. The tibia or shinbone connects the knee to the ankle. The patella (kneecap) is the small bone in front of the knee and rides on the knee joint as the knee bends. The fibula is a shorter and thinner bone running parallel to the tibia on its outside. The joint acts like a hinge but with some rotation.
The knee is a synovial joint, which means it is lined by synovium. The synovium produces fluid lubricating and nourishing the inside of the joint.
Articular cartilage is the smooth surfaces at the end of the femur and tibia. It is the damage to this surface which causes arthritis.
Read on to find out more about Orthopedic Surgery near Bellaire, Houston, TX.
Knee Anatomy
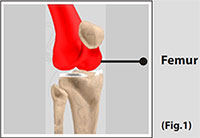
Femur
Femur The femur (thighbone) is the largest and the strongest bone in the body. It is the weight-bearing bone of the thigh. It provides attachment to most of the muscles of the knee.
(Refer fig. 1)
Condyle
The two femoral condyles make up for the rounded end of femur. Its smooth articular surface allows the femur to move easily over the tibial (shinbone) meniscus.
(Refer fig. 2)

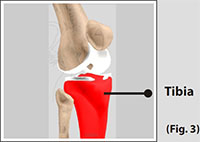
Tibia
The tibia (shinbone) the second largest bone in the body is the weight bearing bone of the leg. The menisci incompletely cover the superior surface of the tibia where it articulates with the femur. The menisci act as shock absorbers, protecting the articular surface of the tibia as well as assisting in rotation of the knee.
(Refer fig. 3)
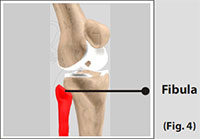
Fibula
The fibula, although not a weight bearing bone, provides attachment sites for the Lateral Collateral Ligaments (LCL) and the biceps femoris tendon. The articulation of tibia and fibula, also allows a slight degree of movement, providing an element of flexibility in response to the actions of muscles attaching to the fibula.
(Refer fig. 4)
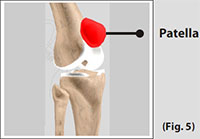
Patella
The Patella (kneecap), attached to the quadriceps tendon above and the patellar ligament below, rests against the anterior articular surface of the lower end of the femur and protects the knee joint.
The patella acts as a fulcrum for the quadriceps by holding the quadriceps tendon off the lower end of the femur.
(Refer fig. 5)
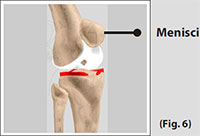
Menisci
The medial and the lateral meniscus are thin C-shaped layers of fibrocartilage, incompletely covering the surface of the tibia where it articulates with the femur. The majority of the meniscus has no blood supply and for that reason, when damaged the meniscus is unable to undergo the normal healing process that occurs in the rest of the body.
In addition, meniscus begins to deteriorate with age, often developing degenerative tears. Typically, when the meniscus is damaged, the torn pieces begin to move in an abnormal fashion inside the joint.
The menisci act as shock absorbers, protecting the articular surface of the tibia as well as assisting in rotation of the knee. As secondary stabilizers, the intact menisci interact with the stabilizing function of the ligaments and are most effective when the surrounding ligaments are intact.
(Refer fig. 6)
Indications for Total Knee Replacement
Arthritis
Arthritis is a general term covering numerous conditions where the joint surface or cartilage wears out. The joint surface is covered by a smooth articular surface that allows pain free movement in the joint. This surface can wear out for a number of reasons; often the definite cause is not known.
When the articular cartilage wears out the bone ends rub on one another and cause pain. There are numerous conditions that can cause arthritis and often the exact cause is never known. In general, but not always, it affects people as they get older (Osteoarthritis).
Other causes include
Trauma (fracture)
Increased stress e.g., overuse, overweight, etc.
Infection
Connective tissue disorders
Inactive lifestyle- Obesity (overweight); Your weight is the single most important link between diet and arthritis as being overweight puts an additional burden on your hips, knees, ankles and feet.
Inflammation (Rheumatoid arthritis)
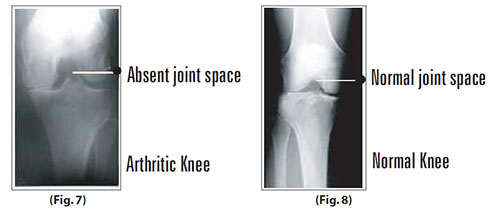
Now compare a normal knee with an arthritic knee.
In the arthritic knee there is an absent joint space. In the normal knee there is a normal joint space.
(Refer fig. 7 and 8)
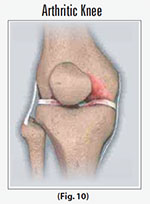
In an arthritic knee
- The cartilage lining is thinner than normal or completely absent. The degree of cartilage damage and inflammation varies with the type and stage of arthritis.
- The capsule of the arthritic knee is swollen.
- The joint space is narrowed and irregular in outline; this can be seen in an X-ray image.
- Bone spurs or excessive bone can also build up around the edges of the joint.
The combinations of these factors make the arthritic knee stiff and limit activities due to pain or fatigue.
(Refer fig. 9 and 10)

Diagnosis
- The diagnosis of osteoarthritis is made on history, physical examination & X-rays.
- There is no blood test to diagnose Osteoarthritis (wear & tear arthritis).
Total Knee Replacement Surgical procedure
Surgery is performed under sterile conditions in the operating theatre under spinal or general anesthesia. You will be lying on your back and a tourniquet applied to your upper thigh to reduce blood loss.
- The surgeon makes an incision along the affected knee exposing the knee joint.(Refer fig. 11)

- The surgeon first concentrates on the femur (thighbone). The damaged portions of the femur are then cut at the appropriate angles using specialized jigs.
(Refer fig. 12 and 13)


- The femoral component is attached to the end of the femur with or without bone cement.
(Refer fig. 14)

-
The damaged area of the tibia (shinbone) and the cartilage are cut or shaved. This removes the deformed part of the bone and bony growth, as well as allows for a smooth surface for which to attach the implants.
(Refer fig. 15 and 16)


-
The tibial component is secured to the end of the bone with bone cement or screws depending on a number of factors and on surgeons choice.
(Refer fig. 17)

-
The surgeon will place a plastic piece called an articular surface between the implants to assure a smooth gliding movement. This plastic insert will support the body’s weight and allow the femur to move over the tibia similar to the original cartilage (meniscus).
(Refer fig. 18)

-
The femur and the tibia with the new components are put together to form the new knee joint.
(Refer fig. 19)

- To make sure the patella (knee cap) glides smoothly over the new artificial knee, its rear surface is prepared to receive a plastic component.
- With all the new components the knee joint is tested through its range of motion.
- All excess cement will be removed. The entire joint will be irrigated or cleaned with a sterile saline solution. The knee is then carefully closed and drains usually inserted and the knee dressed and bandaged.
Risks and complications of Total Knee Replacement
- As with any major surgery there are potential risks involved. The decision to proceed with the surgery is made because the advantages of surgery outweigh the potential disadvantages.
- It is important that you are informed of these risks before the surgery takes place.
Complications can be medical (general) or local complications specific to the knee.
Medical complications include those of the anesthetic and your general well being. Almost any medical condition can occur so this list is not complete. Complications include
- Allergic reactions to medications
- Blood loss requiring transfusion with its low risk of disease transmission
- Heart attacks, strokes, kidney failure, pneumonia, bladder infections
- Complications from nerve blocks such as infection or nerve damage
- Serious medical problems can lead to ongoing health concerns, prolonged hospitalization or rarely death.
Local complications
- Stiffness in the knee: Ideally your knee should bend beyond 100 degrees but on occasion the knee may not bend as well as expected. Sometimes manipulations are required; this means going back to the OR under anesthesia where the knee is bent for you.
- Wound irritation or breakdown: The operation will always cut some skin nerves so you will inevitably have some numbness around the wound. This does not affect the function of your joint. You can also get some aching around the scar. Vitamin E cream and massaging can help reduce this.Occasionally you can get reactions to the sutures or a wound breakdown which may require antibiotics or rarely further surgery.
- Infection: Infection can occur with any operation. In the knee this can be superficial or deep. Infection rates are approximately 1%. If it occurs, it can be treated with antibiotics but may require further surgery. Very rarely your knee prosthesis may need to be removed to eradicate the infection.
- Blood clots (Deep Venous Thrombosis): These can form in the calf muscles and can travel to the lung (Pulmonary embolism). These can occasionally be serious and even life threatening. If you get calf pain or shortness of breath at any stage you should notify your surgeon.
- Damage to nerves or blood vessels: Also rare but can lead to weakness and loss of sensation in part of the leg. Damage to blood vessels may require further surgery if bleeding is ongoing.
- Wear: The plastic liner eventually wears out over time, usually 10 to 15 years, and may need to be changed.
- Cosmetic Appearance: The knee may look different than it was because it is put into the correct alignment to allow proper function.
- Dislocation: An extremely rare condition where the ends of the knee joint lose contact with each other or the plastic insert can lose contact with the tibia(shinbone) or the femur (thigh bone).
- Patella problems: Patella (knee cap) can dislocate. That is, it moves out of place and it can break or loosen.
- Ligament injuries: There are a number of ligaments surrounding the knee. These ligaments can be torn during surgery or break or stretch out any time afterwards. Surgery may be required to correct this problem.
- Fractures or breaks in the bone can occur during surgery or afterwards if you fall. To fix these you may require surgery.
Although every effort has been made to explain the complications there will be complications that may not have been specifically mentioned. A good knowledge of this operation will make the stress of undertaking the operation easier for you to bear.
The decision to proceed with the surgery is made because the advantages of surgery outweigh the potential disadvantages. It is important that you are informed of these risks before the surgery.
You must not proceed until you are confident that you understand this procedure, particularly the complications. Dr. Berkman can help you with the proper assesment from his practice in Bellaire, TX.
Inflammatory Arthritis
Occasionally arthroscopy is used in inflammatory conditions (e.g. Rheumatoid Arthritis) to help reduce the amount of inflamed synovium (joint lining) that is producing excess joint fluid. This procedure is called a synovectomy. After the surgery a drain is inserted into the knee and patients generally require one or two nights in the hospital.
Bakers cysts
Bakers cysts or popliteal cysts are often found on clinical examination and ultrasound / MRI scans. The cyst is a fluid filled cavity behind the knee and in adults arises from a torn meniscus or worn articular cartilage in the knee. These cysts usually do not require removal as treating the cause (torn knee cartilage) will in most cases reduce the size of the cyst. Occasionally the cysts rupture and can cause calf pain. The cysts are not dangerous and do not require treatment if the knee is asymptomatic.
Autologous Chondrocyte Grafting
Isolated areas of articular cartilage loss can be repaired using cartilage transplant technology. This is a new and exciting field that is developing in the treatment of specific isolated cartilage defects in younger patients.
The process is called Autologous Chondrocyte Grafting. It involves harvesting cartilage cells from the affected knee, sending these cells to a laboratory and then culturing the cells to multiply into many cells. The large amount of cells produced are then placed back into the affected knee into the defect requiring resurfacing. Results are still short-term but are looking encouraging.
After a major cartilage or ligament injury has been treated the knee can return to normal function. There is however a small increase in the risk of developing long-term wear and tear (Osteoarthritis) and depending on the degree of injury activity modification may be required.
Activities that help prevent knees deteriorating quickly include:
- Low impact sports like swimming, cycling and walking
- Reducing weight and maintaining a healthy diet
If you are looking for Orthopedic Surgeon that covers the Houston TX, Bellaire TX and Sugar Land TX areas, don’t hesitate to contact Dr. Berkman.
